Hypermobility
- Hypermobility is common in healthy children. The term reflects an increase in range of movement and can be widespread or affect a small number of joints.
- Hypermobility is more common in young children, females and certain ethnic populations (e.g., non-Caucasian children are generally more flexible than age-matched Caucasian children).
- Many children will have no significant difficulties and it can be an advantage in certain situations (e.g., dancing, gymnastics).
- A family history of hypermobility is common.
- Hypermobility can present with the following:
- Joint and muscle pain +/- transient joint swelling.
- Clicking joints.
- Fatigue.
- Hand writing problems*.
- Reduced co-ordination and balance*.
- Flat feet.
- Reduced general activity and function
*If these are predominant concerns then consider Developmental Co-ordination Disorder (DCD)
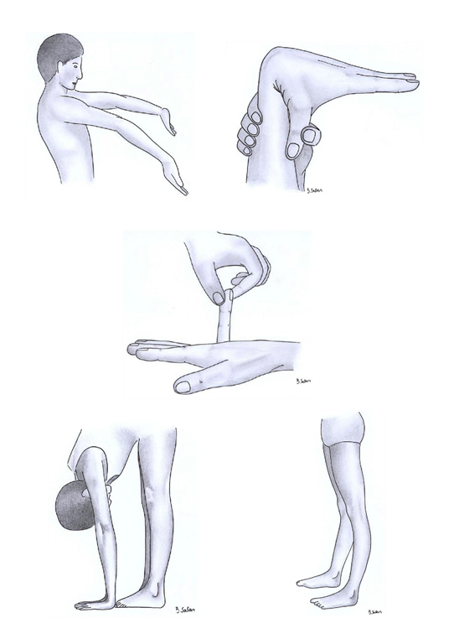
- Examination should include assessment of all joints (e.g., pGALS) where hypermobility is easily observed. e.g., hyperextension of fingers (pictures below), elbows or flat feet.
- A knowledge of normal ranges of movement is useful.
The pictures below demonstrate Hypermobility - Hyperextension of elbows, thumb fully against the forearm, little finger, hands flat on the floor with spine flexed and hyperextension of the knees
- Hypermobility is also a feature of the inherited collagen disorders - these are rare diseases which can cause complications in other systems e.g., cardiac and ocular. It is important to consider these as part of your differential diagnosis:
- Ehlers Danlos Syndrome (easy bruising, stretchy skin and paper thin scars)
- Marfans Syndrome (tall stature, long fingers, wide arm span and high arched palate, scoliosis)
- Osteogenesis Imperfecta (blue sclerae)
- Management - Explanation and reassurance are important and often will suffice, with advice to maintain sporting activities and ensure good muscle strength and endurance with core stability optimised. Occasionally, advice from a paediatric physiotherapist can be useful, particularly in children struggling to return to normal activities, and especially if there is a history of recurrent dislocations.
-
Patient information:
The photograph below shows blue sclerae suggesting osteogenesis imperfecta

The photograph below shows a paper thin scar in Ehler's Danlos syndrome

The photograph below shows elastic skin in Ehler's Danlos syndrome

Indications for concern and specialist opinion include:
- Suspicion of inherited collagen syndromes (e.g., Marfans').
- Pain and functional limitation.
- Asymmetrical hypermobility.
- Inflammatory joint or muscle disease is suspected (remember children with arthritis may also have hypermobility!)
- Recurrent dislocations.

