NSAIDS & Pain Relief
Non-steroidal anti-inflammatory drugs (NSAIDs)
- NSAIDS are recommended for short term use only during flares of joint symptoms. They are useful in reducing inflammation and pain. They can be given prior to school or activity to reduce the need for additional doses at school.
- NSAIDs are better tolerated in children with less side effects (gastrointestinal symptoms).
- Paracetamol / Acetaminophen can be given in combination with NSAIDs.
- Where possible use of tablets or sugar-free preparations are recommended to reduce the risk of dental caries. An electric toothbrush may help protect oral health.
- NSAIDS are not disease modifying but are useful in the short term for symptom relief. If pain continues to be reported then further specialist advice should be sought.
- Aspirin is very useful to treat the arthritis of Acute Rheumatic Fever.
- High Dose Aspirin is used in Kawasaki Disease and helps to reduce aneurysm formation.
Paracetamol (Acetaminophen) and non-opiate analgesics
- These can be helpful with pain control and if used with NSAIDs. Paracetamol is also helpful with fever and is medication that many families are familiar with for childhood intercurrent illnesses.
- Codeine and other non-opiate analgesics are also helpful as pain relief but do cause side effects (e.g., constipation) and need to be used with caution and for short term use.
Non-drug pain relief strategies
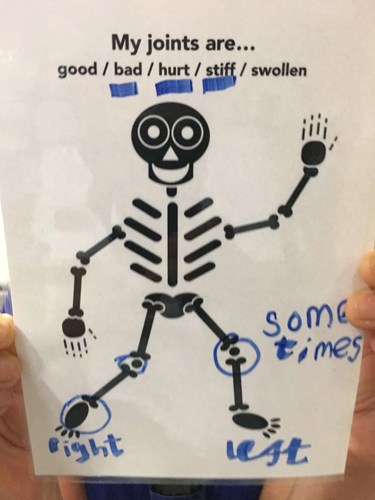
- Pain management starts with a pain assessment. Management differs depending on the cause and type of pain experienced, including the pharmacological strategies used. Chronic/complex pain may need referral to a pain specialist, and ideally needs a multidisciplinary approach.
- Providing an explanation about pain processes and the rationale behind management is important. These explanations should take into account the child/young person’s developmental level and involve the parents/caregivers.
- Pain can be thought of as ‘danger signaling’ and it can be helpful for the child/young person and their family to know whether pain signals should be acted on and how, or whether they are better ignored. Work with the child/young person and family to develop specific strategies. This may need to develop over time rather than be implemented all at once.
- There are many non-pharmacological strategies which play a significant role in pain management, and developing self-management skills:
- Comfort strategies such as cold/warm packs for flares of joint disease, warm showers or baths may help relieve stiffness and also pain, gentle massage.
- Relaxation, breathing, distraction and mindfulness techniques.
- Positive imagery, positive self-talk.
- Pacing and fatigue management, daily and weekly routine and structure.
- Prioritise school when developing participation plans if age-appropriate
- TENS machine - may help with 'background' pain control.
- Distraction techniques - help with procedures e.g., subcutaneous injections and blood tests.
- Pain management plans may need to change to meet changing pain needs and developing cognitive ability.
Nurses have an integral role to assess and manage pain. Key points for good practice include:
- Record a pain history and ensure adequate analgesia as prescribed.
- Observe for signs of pain - verbal, non-verbal and physiological.
- Use an age appropriate pain tool and document results in nursing notes.
- Record pain score regularly and act upon the results.
- Administer analgesia and record age appropriate pain score to assess effect.
- Observe for side effects of analgesia and contact doctor as appropriate.
- Reassure patient and family.