Care pathways
Children with JIA often have a complex pathway to care and may present in various ways to primary or secondary care.
Common presentations include:
- Limp.
- Functional difficulties (such as walking, handwriting, playing sport).
- Joint pain and swelling.
Very young children may not verbalise symptoms and rather than complain of pain, may present with limp, regression of milestones such as walking, ability on stairs or avoidance of activities that they previously enjoyed. Being prone to falling or 'clumsy' are clearly non-specific and may have other causes but a change in ability is important and inflammatory joint disease should be considered.
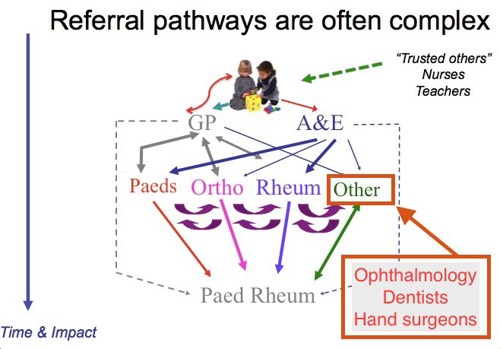
There are many key players, in nursing, health visiting and school health who may notice change and are key to facilitate referral to medical care to establish a diagnosis.
School nurses, teachers and nursery workers may notice change (handwriting, play, sport, general well-being, pain).
School nurses may be alerted to change (well-being, fatigue, physical abilities, pain).
Children may also present to the dentist (with jaw problems), the eye specialist (ophthalmologist, with uveitis and eye symptoms), orthopaedic or hand surgeon (deformity, pain or functional limitation) or to a paediatrician (with fever, rash and joint pain).
If Juvenile Idiopathic Arthritis (JIA) is suspected, then referral to a paediatric rheumatology team for specialist assessment should NOT be delayed.
Early referral to specialist teams facilitates prompt treatment and prevention of complications including joint damage, contractures, and disability.
Many children will do very well on treatment and will go into disease remission.

