JIA Subtypes - Overview
Oligoarticular Onset JIA (70% of cases)
Oligoarticular Onset JIA is the most common form of JIA (70% of cases), typically, pre-school girls with single knee or ankle involvement. Overall it carries the best prognosis - if diagnosed and treated early. There is a high risk of asymptomatic uveitis, which can, if undetected, result in visual loss from cataract and keratopathy (proteinaceous deposits over the eye) - early uveitis is invariably without symptoms - i.e., the eye is not red or painful and there is no blurring.
Bloods tests including rheumatoid factor and radiographs are often normal. The presence of antinuclear antibodies is not diagnostic but is a risk factor for uveitis. Management involves use of intra-articular corticosteroid injections and physiotherapy. Early intervention avoids leg-length discrepancy and muscle wasting. Methotrexate is recommended in patients with severe uveitis, arthritis of a critical joint (such as wrist, temporomandibular joint) or in those children who progress to develop a polyarthritis (referred to as extended oligoarticular JIA) and is observed in 1/3 of those with oligoarticular onset JIA - predicting which children will progress can be challenging.
The photograph shows swollen ankles in oligo-articular JIA.

The photograph below shows keratopathy as a result of chronic anterior uveitis.

Psoriatic Arthritis
Psoriatic Arthritis may present with different patterns - Oligo-articular or Polyarthritis or Enthesitis related - and uveitis is common. Patients may or may not have skin disease at presentation. The diagnosis is suggested by family history, dactylitis (‘sausage digit’), nail pitting, and small joint involvement (hands or feet), which is often asymmetrical (especially the involvement of distal interphalangeal joints). Joint injections, methotrexate and increasingly, biologics are used to treat both joint and skin disease.
The photograph shows asymmetrical involvement of the fingers with a restricted distal interphalangeal joint (ring finger) - this is typical of Juvenile Psoriatic Arthritis.

The photograph below shows nail pitting.

The photograph below shows asymmetrical small joint involvement in the hands - asymmetrical small joint involvement is typical in Juvenile Psoriatic Arthritis.

The photograph below shows dactylitis (sausage digit) in psoriatic arthritis.

Enthesitis-Related Arthritis (ERA)
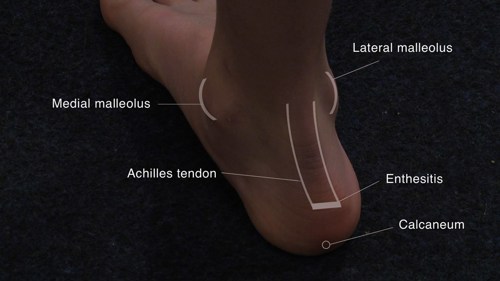
Enthesitis-Related Arthritis (ERA) typically occurs in older boys (>8 years old), who are HLA B27 positive, and may have enthesitis with an oligoarthritis of the knee or ankle or hip. There is an overlap with inflammatory bowel disease. Those that carry HLA B27 are more prone to develop low back involvement (sacroiliitis) and ankylosing spondylitis in later life and a red eye from uveitis (which is different to the chronic anterior uveitis observed most commonly in JIA) - this is acute uveitis with a painful red eye. Management involves joint injections, methotrexate to treat the peripheral arthritis, and biologics are increasingly used. ERA patients often have problems into adulthood.
Polyarticular JIA (20% of cases)
Polyarticular JIA (20% of cases) typically presents with symmetrical arthritis (small and large joints) and in adolescent girls, and follows a course similar to that of adult rheumatoid arthritis, with positive rheumatoid factor, skin nodules, erosive arthritis and an association with HLA DR4. Early introduction of methotrexate, often given parenterally, is advocated. Many patients require use of biologics, often in combination with methotrexate.
The photograph shows polyarthritis of the hands and wrists.

The photograph below shows swollen small joints of the hand and a rheumatoid nodule at the elbow.

Systemic Onset JIA (10% of cases)
Systemic Onset JIA is the least common (10% of cases) subtype of JIA but often follows a severe course with severe polyarthritis and can develop life-threatening complications such as carditis, macrophage activation and sepsis with the infection risk being compounded by systemic immunosuppression. Systemic JIA is characterized by an acute illness with systemic features, fever (quotidian i.e., daily fever spikes - usually late evening to early morning and normal or below normal in between spikes), maculopapular rash (which may appear at times of fever), serositis, lymphadenopathy, hepatosplenomegaly, and high acute-phase reactants and serum ferritin. The systemic features can predate the arthritis by several weeks and these children, who are often very young, are often very unwell. The differential diagnosis includes infection and malignancy (such as leukaemia or neuroblastoma). Treatment includes aggressive use of systemic corticosteroids (often given intravenously during the acute systemic illness), high-dose parenteral methotrexate, and biologics (IL-1 and IL 6 blockade appear to be more effective than TNF inhibitors). Refractory disease may be considered for autologous haematopoietic stem-cell rescue.
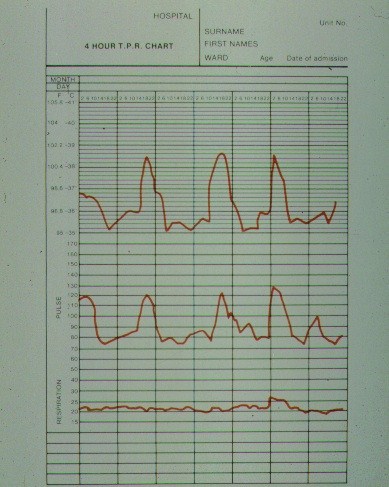
The chart below shows the typical fever chart in systemic onset JIA - the fever often occurs in the evening and the rash may appear at times of fever. The fever tends to return to normal in between.