Common fractures in children
DISTAL RADIAL FRACTURE:
- Most common fracture in children.
- Follows a simple fall – most common mechanism.
- Mostly in the region of metaphysis than involving the physis.
- Torus fracture - Buckle fracture is the most common pattern.
The usual mechanism is a fall on the outstretched hand with the wrist in extension. This compresses the extensor side of the cortex dorsal and tenses the flexor (volar) side of the bone. When the dorsal cortex breaks under compression and the other (volar) remains intact, this pattern is then called a ‘Torus’ fracture. (tori - in Latin means compression).
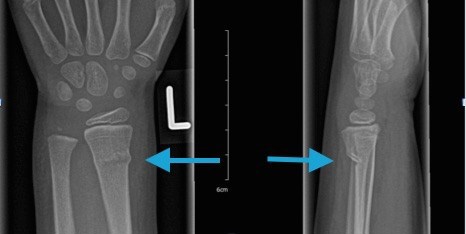
The radiograph below shows a distal radius fracture (arrowed)
- Greenstick fracture – when the incomplete deformation or partial break occurs on the tension side of the bone – here it would be the volar cortex; usually occurs in mid-shaft.
- If the fracture involves the physis, then Salter-Harris type II is the most common pattern.
- Controversies exist in the acceptable angles of deformities around the distal radial physis. Generally, if the child is more than 10 years of age, even minor degrees e.g., 15° or more of angulation is not acceptable.
SUPRACONDYLAR FRACTURE:
- Most common fracture (> 50% of fractures) around elbow in children
- They are important to recognise and treat promptly and appropriately because of the potential to vascular (brachial artery) or nerve injury (most commonly Anterior Interosseous Nerve) or both. They are also notorious to malunite (progressive deformation after union) posing late problems.
- There are two types - Extension (more than 90%) and Flexion – depending on the position of the distal fragment relative to the humeral shaft.
- Displaced supracondylar fractures without any obvious nerve or vessel injury should be manipulated and fixed with K wires, taking care not to cause iatrogenic injury to the nerves (especially the ulnar nerve).
- Brachial arterial injury can also occur, although rarely, following reduction of a supracondylar fracture by closed methods.
- A child presenting with traumatic elbow swelling should be assessed immediately for capillary refill, distal neurovascularity and a Plaster of Paris (POP) back slab applied in the same resting position of the elbow.
- Manipulation of the elbow should never be attempted while placing the initial POP back slab.
The radiograph below shows a supracondylar fracture (arrowed) and the insertion of K wires after manipulation.

MID-SHAFT FOREARM FRACTURE:
- These fractures involve the diaphyses of the radius and ulna.
- Mechanism is fall on to extended wrist and extended elbow.
- Almost half of them are Greenstick fractures.
- The classic treatment for these Greenstick fractures is to ‘complete’ the fractures under general anaesthetic and application of an above elbow cast.
- Manipulation to reasonable apposition of the displaced bones is usually sufficient.
- Rotational alignment is the most difficult to achieve, sometimes due to inherent plastic deformation.
- The fractures have to be reduced internally by surgery when there is:
- Failure to reduce by closed methods due to soft tissue interposition.
- Evidence of open fractures.
- Failure to maintain reduction (If the reduction slips out in cast, on check radiographs taken within a week).
- The usual choice of fixation in paediatric forearm fractures is flexible intramedullary nails that are introduced percutaneously and removed at a later date.
The radiograph below shows a mid-shaft fracture (arrowed)

GALEAZZI FRACTURE:
- The distal radio-ulnar joint dislocates with a fracture occurring at the junction of distal 1/3rd and middle third of radius.
- This pattern is always fixed internally in adults, whereas in children a closed long arm cast for six weeks would suffice after reduction under general anaesthetic.
The radiograph below shows a Galeazzi fracture (arrowed)


