Mimics of Arthritis
- A Mimic of Arthritis refers to conditions that are not rheumatological (i.e., not Juvenile Idiopathic Arthritis (JIA).
- The term 'musculoskeletal conditions' includes many pathologies from rheumatology, orthopaedics, neurology, metabolic medicine and clinical genetics as well as the spectrum of normal development (e.g., hypermobility, normal variants).
- Careful clinical assessment, family history (including any evidence of consanguinuity), birth history and presence or absence of red flags are most important when considering the differential diagnosis.
- The use of investigations and their judicious interpretation will help to confirm or refute potential causes and especially those requiring urgent medical intervention.
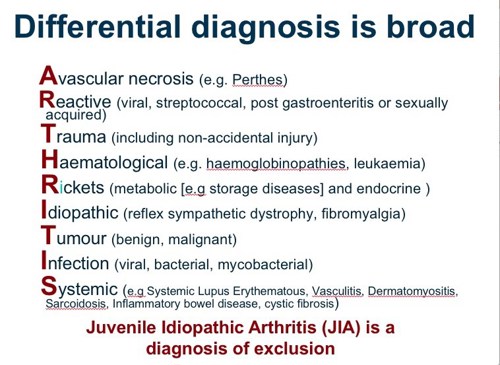
- Leukaemia or lymphoma or neuroblastoma can cause widespread arthralgia and sometimes arthritis along with bone pain and night waking. The 'unwell child' with systemic features and / or cytopenias must always raise concerns about malignancy. There needs to be a low threshold for a specialist opinion and bone marrow aspiration.
- Bone cancer must be considered with refractory joint or bone pain especially with night pain and in sites where bone tumours are most common - e.g., distal femur and proximal tibia. Coexistent joint swelling can occur with bone cancers and so if there is suspicion then imaging of long bones above and below the joint e.g., the knee.
- Infections (e.g., Arboviruses and Acute Rheumatic Fever - ARF) and some forms of reactive arthritis cause multiple joint arthralgia or reactive arthritis. ARF tends to affect multiple joints although a monoarthritis is also possible.
- Inherited neuropathies and neuromuscular diseases must be considered in the child with delayed motor milestones. In contrast, inflammatory joint or muscle disease tend to cause regression of motor milestones.
- Congenital bone and joint deformities may not be apparent at birth (e.g., developmental dysplasia of the hip or birth trauma resulting in nerve palsy) and may become more obvious as the child becomes more active.
- Children with genetic or chromosomal conditions (such as Downs syndrome) may be prone to developing a spectrum of joint problems, ranging from hypermobility to inflammatory arthritis. Functional problems may be falsely regarded as being due to the underlying genetic or chromosomal condition and inflammatory arthritis may be missed.
- Inherited metabolic conditions (including mucopolysaccharidoses) may manifest with complex multisystem involvement including joint restriction (due to contractures or abnormal skin thickening) and / or joint laxity / hypermobility.
- Skeletal dysplasias may result in bone or joint pain and deformity in the absence of synovitis. They are suggested by other features such as short stature, joint contractures and family history.
- Single joint arthritis mimics include infection - especially Tuberculosis - which must always be suspected in endemic areas and with coexistent Human Immunodeficiency Virus Infection.
- Sickle cell disease causes acute joint pain and swelling, usually small joints in the hands and feet, often with soft tissue swelling (dactylitis - sausage digit) and may be suggested by family history.
- Localised Idiopathic pain syndromes can be suggested by severe pain with marked functional dysfunction in the absence of any indication of overt musculoskeletal pathology.

