Physeal injuries
The type of injury pattern is helpful to determine prognosis.
The most widely used classification system for physeal injuries is that of Salter-Harris (below):
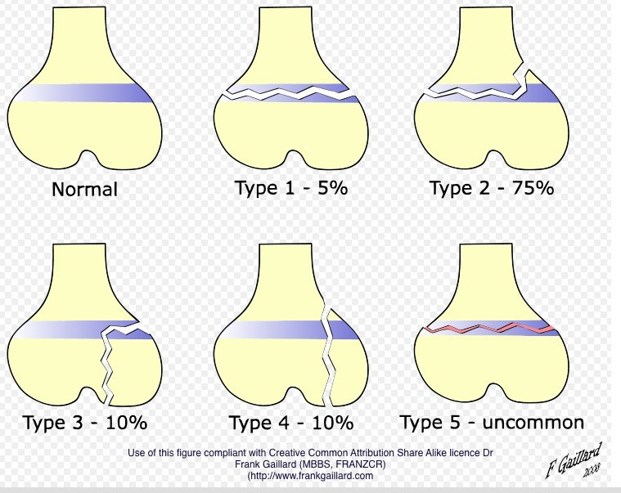
- Type I is a physeal separation without any bony injury.
- Type II has a metaphyseal extension – most common.
- Type III extends into the epiphysis (Intra-articular).
- Type IV has a fracture line that extends from the epiphysis through the physis to the metaphysis.
- Type V injuries carry the worst prognosis as the entire physis gets compressed, without any visible fracture lines.
Combinations of these patterns are also common, necessitating the evolution of other classification systems. For example the Tillaux fracture in the adolescent ankle has both type II and type III injuries in different planes.
The usual treatment for types I to IV are manipulation with (usually) or without fixation with temporary wires (designed by Kirschner – “K wires”) or using partially threaded screws (in large fragments / adolescents).
Acute injuries must be immobilised in an incomplete Plaster of Paris cast, called the ‘back-slab’, so as to allow some swelling from the fracture. Completed casts for acute injuries, tight casts, casts that are not moulded well or casts that have constriction rings can cause a dreadful entity called Compartment Syndrome, reducing the circulation and tissue perfusion in that affected limb.
The first treatment in suspected cases of compartment syndrome is to split the cast open down to the skin and elevation. Fracture positions or losing reduction is a negligible complication in these scenarios.
Fractured limbs must be immobilised and maintained in elevation to aid venous drainage and reduce swelling, thereby pain.
Upper limbs: Broad arm slings, Bradford Slings or simply pillows where appropriate.
Lower limbs: Braun frames, pillows or simply foot-end elevation of the bed.
Injuries of and around the growth plate (physis) are managed with lower threshold for surgical manipulation (mobilising the fracture ends under general anaesthetic) and reduction (opposing the fracture ends). An exception to the rule is management of proximal humeral injuries (1% of childhood fractures), where the remodelling potential is the greatest and so most are managed without surgery.
If there is a significant injury to a segment of physis, that segment stops growing, termed as growth arrest. The rest of the physis has a normal growth pattern resulting in a deformity. Growth arrest can be complete or partial. Complete growth arrest results in leg length discrepancy. Partial arrests can result in angular deformity or joint incongruity. Therefore surgically stopping the ‘normal’ growth of normal physis, at accurately calculated times, prevents say, an angular or a shortening deformity. There are skeletal predictive growth charts and tables available to predict the growth pattern and time the surgery.

