Bone Disease
Bone disease may be investigated by:
- Blood tests - serum calcium, phosphate, alkaline phosphatase and 25-hydroxy-vitamin-D (25-OH-vit-D) and parathyroid hormone (PTH), vitamin C and uric acid blood tests.
- Imaging (radiographs) - for evidence of skeletal dysplasia
- Bone density (DXA) - densitometry is most commonly used to assess bone density, with adjustment needed for skeletal size. Sequential measurements (usually 2 yearly) are used to monitor progress. It is important for paediatricians to be familiar with the interpretation of DXA using Z scores (i.e., matching for age and gender normal values).
- Genetic testing - collagen genes.
Examples of bone diseases are described below:
Osteomalacia / Rickets - In young children, Vitamin D deficiency presents with failure to thrive, limp, aches and pains, bow legs and myopathy (proximal weakness). A dietary history is important (e.g., milk ingestion, duration of exclusive breastfeeding, formula milk) and sun exposure.
Primary osteoporosis - Osteogenesis imperfecta (OI) consists of a group of inherited abnormal collagen conditions, resulting in abnormal type 1 collagen (the major protein found in bones, ligaments and tendons). This manifests as bone fragility, with bowing, low trauma fractures and hypermobility. In the most common form (type I), which is autosomal dominant, there are fractures during childhood, often after minor trauma, and a typical blue appearance to the sclerae is present. Some children develop hearing loss and may have abnormal teeth. Treatment with bisphosphonates reduces fracture rates. There is a severe, lethal form (type II) with multiple fractures which occur before birth and many infants are stillborn; inheritance is autosomal recessive or due to new mutations.
Secondary osteoporosis - occurs in any inflammatory chronic condition (e.g., Juvenile Idiopathic Arthritis) and may increase fracture risk, often after low trauma. The use of glucocorticoids may increase fracture risk, especially with prolonged use at high doses. Other chronic conditions which result in prolonged immobility and disuse atrophy - such as Duchenne muscular dystrophy – can cause decreased bone mass - the effects can be exacerbated with use of glucocorticoids. Endocrine problems such as anorexia nervosa, thyroid disease and Turner’s syndrome can cause osteopenia and osteoporosis. Chronic liver and kidney diseases may also cause osteoporosis.
Other rare metabolic diseases as juvenile gout can also cause bony erosions and deformities. Scurvy caused by prolonged severe dietary deficiency of vitamin C may be responsible of osteopenia. Undernutrition, particularly protein undernutrition contributes also to the occurrence of osteoporosis.
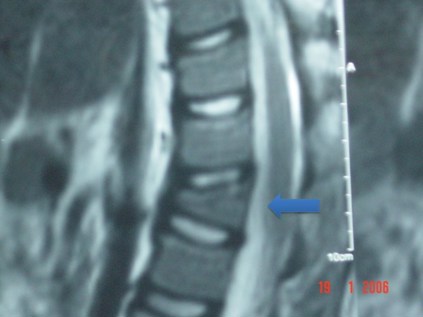
The MRI below shows vertebral collapse (see arrow pointing to an abnormally wedge-shaped vertebral body) due to osteoporosis.
Skeletal Dysplasias - these present with bone pain or joint deformity such as swelling. They may be suggested by short stature, joint contractures and pain often with a positive family history. Achondroplasia is one example of a skeletal dysplasia and may present with short stature, and disproportionate short limbs to trunk (figure below).

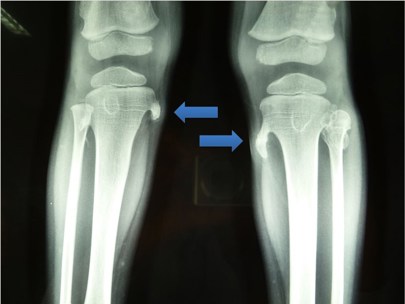
The radiographs demonstrate bone exostoses (blue arrows) on the medial tibiae due to skeletal dysplasia. These will be felt as hard lumps and are usually not tender.
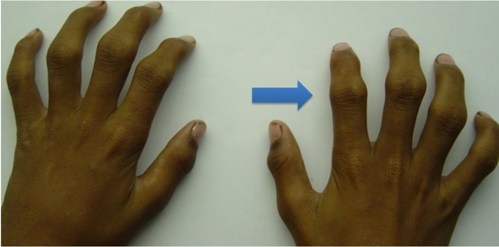
The photograph below shows symmetrical bony swelling and deformity in a skeletal dysplasia called pseudorheumatoid dysplasia.
The photograph below shows short big toes due to a rare skeletal dysplasia called Fibrous Ossificans Progressiva.


