Swollen Toe
Nehal is a 10 year old boy who presents with a swollen toe to the emergency department.
He is a keen soccer (football) player but cannot recall any injury. Otherwise he is well with no systemic features to suggest red flags in the history and the examination is otherwise reported as normal from the emergency department assessment. He has a swollen toe ('sausage like').
Investigations - radiograph shows no fracture. Ultrasound shows soft tissue swelling and effusion in the interphalangeal joint and metatarsal joint. Full [complete] blood count, acute phase reactants normal. Autoantibodies are normal. He is referred to orthopaedics who perform aspiration of the toe joint under anaesthetic. Cultures are negative but he has a six week course of antibiotics. At review, he is no better and now has pain in his fingers. He is referred to paediatric rheumatology. pGALS demonstrates small joint involvement in his fingers and nail pitting. There is a family history of psoriasis (father).
This is Juvenile Psoriatic Arthritis.
Management: Joint injections under anaesthetic. He was started on methotrexate and folic acid. He was taking NSAIDs for pain relief. He has input from the multidisciplinary team with education about his condition and treatment. He is referred for physiotherapy and occupational therapy. Eye screening shows no evidence of uveitis. Subsequent blood tests show that he is HLA-B27 positive.
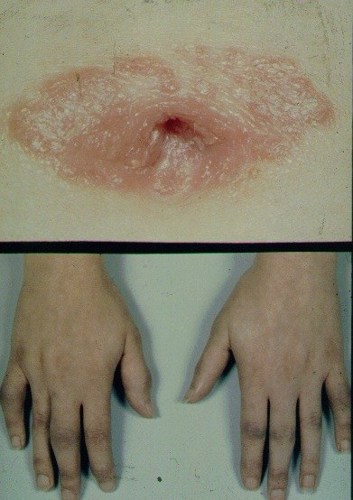
The photograph shows umbilical psoriasis and asymmetrical arthritis in psoriatic arthritis.
The presence of HLA-B27 is common in many healthy people.
In the presence of inflammatory arthritis, it can associate with axial spine involvement (which may present later on with pain / stiffness in the neck or lower back) and acute uveitis (which will cause a painful red eye and is different to the chronic anterior uveitis observed in many cases of JIA). This has implications for monitoring and eye screening.

