JIA Associated Uveitis and eye screening
- Uveitis is the term for intraocular inflammation of those layers internal to the sclera and cornea.
- The term uveitis refers to inflammation of the uveal tract (vascular layer including the choroid, ciliary body and iris) but can also refer to inflammation of the retina and vitreous.
- JIA is the commonest systemic disease associated with uveitis and affects 15% of children with JIA in the literature from Europe and North America. The incidence of uveitis varies elsewhere which may reflect referral bias or true differences in incidence.
- JIA associated uveitis is usually chronic anterior uveitis (CAU) and can occur before, or up to 7 years after the onset of arthritis. CAU is invariably asymptomatic in the early stages (i.e., with no pain, the eye is not red and there is no blurring), can be bilateral and is only detected by eye screening. Once a child develops symptoms (blurring) then outcome is worse. JIA uveitis can cause irreversible blindness if not detected and treated. All patients with JIA require regular eye checked for uveitis screening.
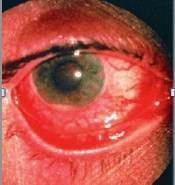
The photograph shows an eye that is blind from cataract and keratopathy
- Uveitis can occur in any subtype of JIA and at any time (even before onset of arthritis) but typically affects young children (under 7 years) with oligoarticular JIA rather than polyarticular onset and those carrying antinuclear antibody (ANA).
- Uveitis is much less common in systemic JIA and chronic asymptomatic anterior uveitis is not typically associated with childhood onset Enthesitis Related Arthritis (ERA) or Rheumatoid factor positive JIA. The presence of psoriasis may increase the risk of chronic anterior uveitis.
- All children with suspected JIA should have eye screening with a slit lamp examination. Screening is required at regular intervals and often for several years as uveitis can occur at any time and be asymptomatic.
- Flares may occur during changes or breaks in systemic treatment. Uveitis can also flare despite arthritis remission.
- Poor prognostic features for visual outcomes include onset of visual symptoms before being detected by screening and uveitis prior to arthritis. Visual loss occurs due to cataract, band keratopathy and glaucoma.
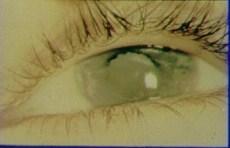
- Children with JIA who carry HLA-B27 (such as in ERA) may develop an acute uveitis with a painful red often photophobic eye; this is rather like acute anterior uveitis that develops in ankylosing spondylitis in adults. Children with HLA-B27 and ERA do not need regular eye screening as they will present with acute uveitis flares.
The photograph below shows acute uveitis in HLA-B27 related ERA - the eye is painful, inflamed, and photophobic.