Limp and a Swollen Joint
Ana is a 2-year old girl referred from a community hospital in South Africa to the local specialist centre as she was not responding to treatment for a presumed 'septic arthritis'. On questioning, she had a 7-month history of limp and swelling of her right knee. Her mother had noticed that she held her leg quite stiffly, more so in the last few weeks and she now refused to weight bear, complaining of pain in her knee. Paracetamol and Ibuprofen helped to control her pain but she was not completely pain free. She had no preceding illness or trauma and there had been no fever, rashes or weight loss noted. She had a normal delivery at term and had normal developmental milestones. She had received the BCG vaccination at birth and all the immunisations appropriate for her age. She had been bottle fed, was on a toddler’s diet but was currently not eating well. Her health record showed that her weight had been maintained between the 25th and 50th centile.
On further enquiry, it was discovered that her mother had been treated for Tuberculosis (TB) 4 years ago and is Human Immunodeficiency Virus (HIV) positive on antiretroviral therapy. Ana was found to be HIV PCR negative at 15 months. Examination on admission revealed an unhappy child, her weight at 12kg (between the 25th and 50th centile), height 85cm (above 25th centile). She had no fever, no palpable lymph nodes and no skin rashes. The respiratory, cardiac and abdominal examination were normal. Joint examination showed a slightly warm swollen knee with a large effusion and limited range of movement (loss of hyperextension and flexion to 60 degrees). No other joints were affected.
Investigations:
- Full blood count: White cell count 14.1 x 109/L, Haemoglobin 11.2g/L Platelets 534 x 109/L.
- Antinuclear antibody negative. Rheumatoid factor negative.
- CRP 18mg/L (normal <5) ESR 34mm/hr (normal < 10). Repeat HIV screen: negative
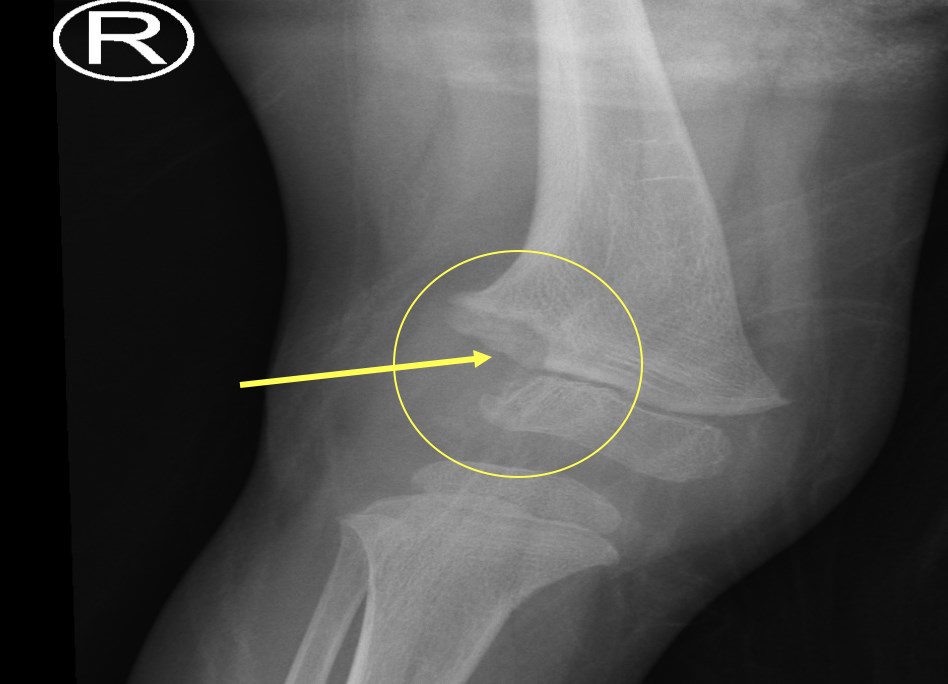
- X-ray of her right knee (below) showed a destructive lesion (arrowed)
- Synovial fluid analysis: Multiple TB microscopy and cultures: negative. TB Gene Xpert (TB PCR assay) of synovial fluid: Negative
- Tuberculin Skin test: was not available
- Synovial biopsy of the knee joint was performed. This showed a chronic synovitis but no granulomas nor malignant cells. A second biopsy was done which was positive for tuberculous granulomas.
A diagnosis of destructive TB arthritis was made. She improved remarkably after commencement of 4 drug TB treatment.
TB mono-arthritis may occur in children who appear otherwise well and often affects a single large joint, most commonly, the hip or knee. It is not an easy diagnosis to confirm and many attempts at finding evidence of the mycobacterium is often necessary. Treatment may be commenced when suspicion is high in endemic areas and the clinical findings do not fit any other diseases in the differential diagnosis. Treatment for TB in bones and joints includes standard four drug regimens for between 6 -12 months. Clinical improvement occurs within a few weeks of starting treatment.
Her presentation would be not be consistent with oligo-articular JIA as she was unwell and the radiographic changes suggested an aggressive process. In a high risk or endemic area for TB (and/or HIV), then the presentation would need to consider TB; TB and HIV often co-exist.
Erythema nodosum (picture below) occurs in some cases of TB and may be helpful in the differential diagnosis.


