Developmental Dysplasia of the Hip
Developmental Dysplasia of the Hip (DDH), replaces the term Congenital Dislocation of the Hip and Neonatal Instability of the Hip. DDH can be present at birth but also develop later in life. Early diagnosis is important, as it leads to improved outcomes.
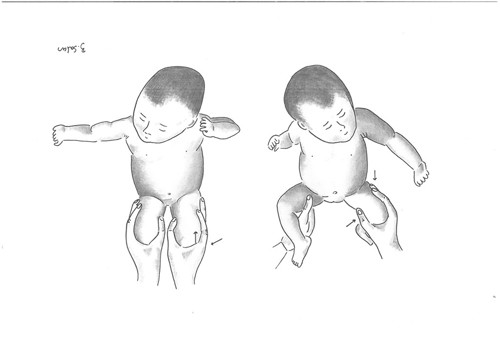
DDH refers to a spectrum of problems with one common feature: insufficient coverage of the femoral head by a shallow and steep acetabulum. In newborns, DDH is often associated with an unstable hip. This ranges from a slightly unstable hip via a dislocatable hip (Barlow positive) to dislocated but reducible hip (Ortolani positive) - images below.
If treated early (within the first month of life) with abduction splints, the prognosis for a normal hip development is excellent. The treatment of DDH becomes more demanding with increasing age of the child, including open reduction, pelvic osteotomies and prolonged treatment with hip spica casts.
DDH affects around 1-3% of all newborns, is 6-9 times more common in girls and 20% are bilateral. Risk factors for DDH include vaginal breech delivery, caesarean breech delivery, oligohydramnios, multiple pregnancy, prematurity, and neuromuscular disorders (e.g., cerebral palsy).
DDH is often detectable at birth, and hence is screened for as part of the newborn check. This is done by performing Barlow’s and Ortolani’s tests, which look for the ability to dislocate and relocate a femoral head respectively. After 2-3 months of age, Barlow’s and Ortolani’s tests become more difficult to perform, due to development of muscle tone, and are therefore unsuitable. In those cases, a limited abduction when the hip is flexed is the most important clinical finding of a dislocated hip. In most infants it should be possible to fully abduct a flexed hip so that the lateral knee touches the examination couch. It is important to assess for asymmetry since most cases of hip dislocation is unilateral.
During the first weeks of life, DDH is diagnosed by clinical findings alone or by the assistance of ultrasound. Two principally different ultrasound investigations are used, either dynamic with the purpose to assess instability, or static with the purpose to assess acetabular dysplasia. In these infants, first line treatment consists of bracing- a harness or splint which must be worn continuously for around 6-8 weeks, being adjusted as the infant grows
Paediatric Orthopaedic surgeons should be involved in the management of DDH.
The radiograph shows a late diagnosed DDH of left hip in a child aged 23 months

After 3 months of age, DDH may be suggested by asymmetrical skin folds, leg length discrepancies, buttock flattening, and walking with the affected leg in external rotation. Older children may present with a gradual onset of a painless limp, tip-toe walking on the affected side, as well as leg length discrepancies. Delay in walking is not commonly seen.
Early diagnosis is important, as it leads to improved outcomes. The majority of unstable hips in neonates resolve spontaneously with 2-6 weeks, and this can be monitored through ultrasound. Wearing an oversized nappy or diaper helps to keep the hips abducted and femoral head in the acetabulum. If they do not resolve, prompt treatment is required. In children <6 months of age, first line treatment consists of bracing - a harness or splint which must be worn continuously for around 6-8 weeks, being adjusted as the infant grows. The aim is to maintain hip reduction. In children >6 months, splinting and reduction may not be suitable and surgery may be required.
Paediatric Orthopaedic surgeons should be involved in the management of DDH.
Further Reading

