Well Child and Leg Pains
Chloe is 8 years old and presents with a 6 month history of leg pains. This would often happen after football and she has now stopped this as an after school activity. She is often reluctant to walk long distances. Her parents comment that she complains of pain ‘a lot’ and more than her older brother does. They have tried giving her paracetamol (acetaminophen) and changing her shoes but her pain has persisted. Chloe’s pain tends to be after exercise and particularly at the end of a school day. Evenings can be difficult. She seems to be fine in the mornings. Parents describe mild, intermittent swelling that resolves spontaneously.
Chloe had a clicky hip at birth but was reassured after a normal ultrasound scan of her hips. She has had no other significant past medical history and is taking no other medications. She walked at 12 months of age. Her development has otherwise been normal although her mother comments that it took her longer to ride a bike compared to her friends.
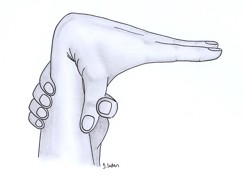
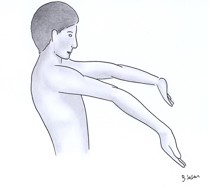
On examination Chloe appeared well with no pallor, rash or lymphadenopathy. pGALS assessment showed generalised hypermobility, marked at her knees and hips. She also had increased flexion at her wrists and at her fingers (as shown in the pictures below). There was no joint swelling and no restricted joint movement. There was no muscle weakness or wasting.
The photographs below show a) hyperextension of the little finger (>90 degrees), b) full flexion of the thumb to reach the forearm, c) hyperextension of the elbow and hyperextension of the knee. These changes are characteristic of hypermobility and should be symmetrical.


This is a typical case of a normally developing child hypermobility.
Pain can be associated with activity and is brought on by muscle fatigue. Often the patient will stop the relevant activity, with a recurrence of the pain whenever the activity is resumed. The above examination findings are typical for hypermobility, but other causes for pain should be considered and excluded.
Further Information
Not at this point in time. There is no history of trauma or inflammatory symptoms. Red flags for systemic disease are absent. Note the history of difficulties with riding a bicycle – be aware of Developmental Co-ordination Disorder (DCD), which may present with clumsiness and difficulty with certain activities.
Further Information
https://www.nhs.uk/conditions/developmental-coordination-disorder-dyspraxia/
Discussion should be targeted to explaining hypermobility and how this should be managed. Reassurance should be given and advice about maintaining muscle strength, improving stamina and returning to physical activities – this may require a gradual return to play and sport. The family and patient should be given information about when to return to seek medical attention again, and particularly about red flag symptoms and worsening pain.
Patient information can be found at the following websites:
Maintenance of activity, fitness and muscle strength is important.
There may be activities that do not trigger pain (such as swimming, cycling), which the patient should be encouraged to try.
A referral to Physiotherapy is appropriate if the usual activities and sports are being avoided.
If handwriting is painful or slow due to hypermobile fingers, a referral to Hand Therapy can be helpful.
Patient information can be found at the following websites:

