Muscle Assessment
- Given the wide differential for muscle disease presenting as weakness, limp or muscle pain, the work-up starts with a thorough history and examination.
- Key features in the history and examination are provided.
- Check for wasting (atrophy), hypertrophy or pseudohypertrophy, fasciculations or tenderness, contraction with percussion (myotonia).
- Check for any skin changes e.g., oedema, erythema, and rash (which may suggest a multisystem disease such as Juvenile Dermatomyositis).
- A neurological assessment is indicated to assess muscle tone, reflexes and cranial nerves - these assessments give valuable information to determine the site of pathology in the neuromuscular system.
- In a child with muscle disease it is important to also assess the vital functions of speech, swallowing and breathing, in addition to gait. Muscle strength in infants is usually based on inspection and assessment of developmental milestones, rather than formal scoring.
- It is also important to assess speech, swallowing and breathing as children may be at risk of aspiration due to bulbar muscle involvement.
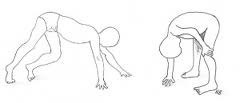
- Proximal weakness may be suspected with a waddling gait or abnormal motor milestones. There may be difficulty or inability to jump. Gower's sign for proximal weakness is demonstrated when a child is asked to get up from being supine on the floor - they will roll onto their tummy and push themselves up using hands on their thighs.
- Delay in walking / motor milestones suggests an inherited myopathy such as Duchenne Muscular Dystrophy.
- Regression in walking / motor milestones is more suggestive of inflammatory muscle disease (such as Juvenile Dermatomyositis) or inflammatory joint disease (such as Juvenile Idiopathic Arthritis).
- The assessor grades the child's ability and strength with an objective score that can be used to measure severity and also to monitor progress. There are several tools available.
- The Childhood Myositis Assessment Scale (CMAS) has been shown to be a valid measure of physical function in children with juvenile idiopathic inflammatory myopathies including Juvenile Dermatomyositis (JDM). The CMAS assesses muscle strength and endurance, includes 14 manoeuvres and is scored to yield a total maximum score of 52.
- MMT8 (Manual Muscle Testing and a subset of Eight Muscles) – a set of 8 designated muscles tested unilaterally to assess muscle strength and also used in the assessment of patients with myositis.
- The following resources are available to demonstrate clinical tools to assess muscles:
- https://www.niehs.nih.gov/research/resources/assets/docs/cmas_instructions_508.pdf - CMAS instructions.
- https://www.niehs.nih.gov/research/resources/assets/docs/cmas_508.pdf - CMAS scoring sheet.
- The PReS Juvenile Dermatomyositis Working Party have collated useful resources to aid muscle assessment using CMAS and MMT. https://www.pres.eu/working-parties/JDM-working-party.html
- The MRC (Muscle Research Council) Muscle Power Grading - also known as the Oxford Scale is outlined below:
|
Grade |
Description |
Power |
|
0 zero |
No visible muscle contraction or movement |
None |
|
1 |
A flicker of muscle contraction but insufficient to cause limb movement |
Minimal |
|
2 |
No limb movement against gravity but complete movement of limb with no gravity i.e., movement in horizontal plane |
Poor |
|
3 |
Complete movement of limb against gravity but no resistance |
Fair |
|
4 |
Complete range of movement against gravity but without full resistance |
Good |
|
5 |
Complete range of movement against gravity with full resistance i.e., normal muscle strength |
Normal |
More Information about muscle disease and limp is available.
More information about the approach to suspected muscle disease is available.
Further information about muscle disease is provided in the clinical cases:
- Frequent Falls - Duchenne Muscular Dystrophy (DMD
- Delayed Walking - DMD
- Fatigue and Muscle Pain - JDM
Further information about muscle disease is available - https://childmuscleweakness.org

